
Tennis elbow is also known as lateral elbow tendinopathy, tendinosis or lateral epicondylitis (in the acute phases). Tennis elbow is characterised by elbow pain on the outside of the bony part of the elbow and often results in grip weakness. This can be due to injury or tendon weakening where the common forearm extensor tendon is located. Common symptoms include:
We have complied a list of common questions we hear in the clinic to assist your understanding of Tennis elbow, the symptoms and available management strategies for your injury.
The common extensor tendon is the primary structure involved in Tennis elbow. This tendon is the shared insertion point for 5 muscles found on the dorsum of the forearm. These muscles are involved in actions of lifting or extending the wrist and fingers, sweeping the wrist from side to side and rotating the forearm. The primary wrist extensor, Extensor Carpi Radialis Brevis, is thought to be involved in most cases of tennis elbow. The common extensor tendon connects these muscles to the outer aspect of elbow joint, on a bony projection called the lateral epicondyle.
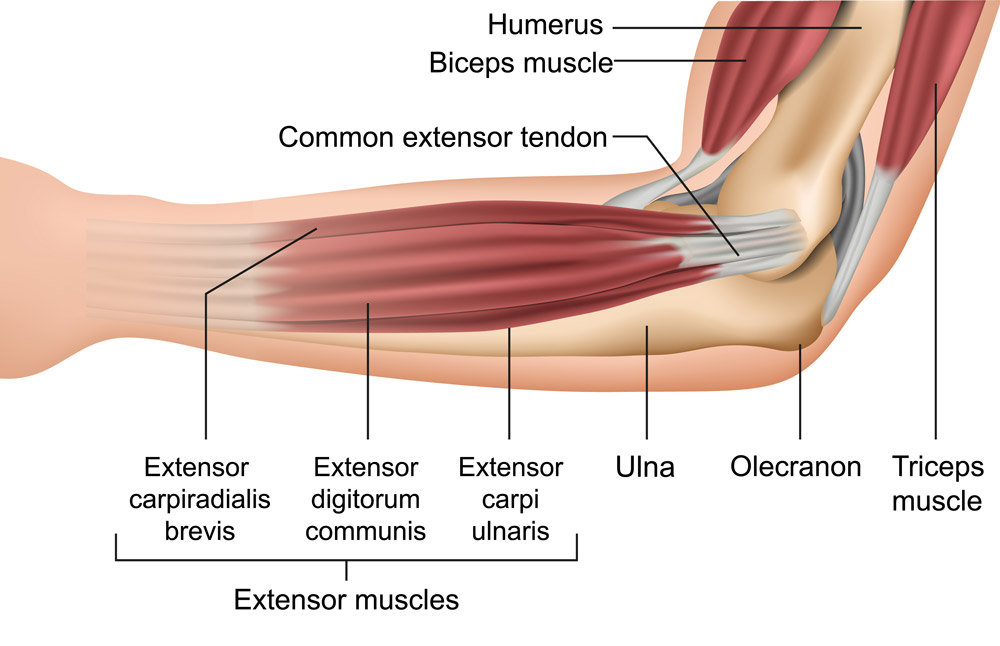
Stress to this common extensor tendon is primarily placed while loading the wrist extensor muscles in a “stretched” position, such as gripping in an extended elbow and palm down posture. Due to this, people who experience tennis elbow may have pain in simple tasks such as reaching for a coffee cup.
The term Tennis Elbow is commonly given for this condition as these aggravating actions are regularly replicated in gripping and swinging a tennis racket, therefore increasing injury risk if a poor technique is being utlised or underlying weakness is present.
A common question we hear in clinic is “why do I have tennis elbow if I don’t play tennis?”
Despite its name, the majority of tennis elbow presentations do not present from tennis players, with 1-3% of individuals aged 30-64 acquiring tennis elbow (Shiri et al., 2006). Tennis elbow is most common in general working populations with an occurrence rate of 2-23% (Shiri et al., 2006). Many day-to-day activities involving gripping results in the great majority of these presentations.
Tennis elbow can develop overtime from repeated hand use; such as cleaning, tool use or sustained use of a computer mouse with a non-ergonomic desk set-up. An acute injury can also cause tennis elbow where the elbow and wrist are rapidly extended, such as losing control of a heavy weight at the gym.
There is pleasing evidence for the great majority (89%) cases being managed within 12 months, with further studies demonstrating effective relief of symptoms via a 6-12 week rehabilitation program (Chen & Barker, 2023). A chronic tendinosis is found to develop in 40% of cases and is more likely to develop without intervention. Generally, tennis elbow does get better. Most cases can take several months with some having a lingering pain for around 18 months to 2 years.
During injury, micro-damage is caused to the tendon. The common extensor tendon has a poor blood supply, meaning that it takes a long time to heal when compared to other body structures such as muscle and bone. As the tendon is the shared insertion point of 5 different muscle groups, it can also be quite difficult to provide adequate rest that is needed to the tendon for healing. Continued aggravation to the site of injury overtime is thought to cause a disruption to the internal architecture of the tendon; causing a disorganisation to internal collagen fibres and cellular change (Eapen, et al., 2023). This progress is called angio-fibroblastic tendinosis. These changes result in further weakening to the tendon if not effectively managed (Eapen, et al., 2023). Thankfully, studies also demonstrate an improvement/re-organisation to these tendon changes if an appropriate rehabilitation program is followed post injury (Cook, & Purdam, 2009; Chen & Barker, 2023).
“Management strategies for tendinopathy indicate that a careful balance between rest and use of the tendon is needed.” (Cook, 2019).
Finding the “just right” level of tendon loading is the first step towards managing symptoms of Tennis elbow. Rest to the injury needs to be carefully matched with an exercise program to re-load the tendon in a tolerated capacity. It can be quite difficult to identify the correct level to commence strengthening or re-loading the arm. We find that many people who have tried prior strengthening programs without success, have commenced exercises that are too advanced for their symptoms.
“Currently, a supervised gradual loading program is the most evidence-based approach to managing tendon pathology.” (Cook, 2019)
If the above strategies do not assist with symptom relief, it is recommended that you gain further professional advice.
A Hand Therapist will assess your injury and ask questions surrounding your lifestyle demands such as work, leisure and daily tasks that may be affecting your injury. We will then apply best practice strategies for managing tennis elbow, catered to your unique presentation. Hand therapists working in the private sector generally see a huge number of people with this condition and therefore keep very up to date with techniques and options for getting you back on track.
Contact us if you would like the expert help to manage your Tennis Elbow symptoms.
References:
Chen, Z., & Baker, N. A. (2021). Effectiveness of eccentric strengthening in the treatment of lateral elbow tendinopathy: A systematic review with meta-analysis. Journal of Hand Therapy, 34(1), 18-28.Retrieved from https://www.sciencedirect.com/science/article/pii/S0894113020300272
Cook, J. L., & Purdam, C. R. (2009). Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British journal of sports medicine, 43(6), 409-416. Retrieved from https://bjsm.bmj.com/content/43/6/409
Eapen, C., Rosita, R., Sohani, M. S., & Patel, V. D. (2023). A systematic review of the effectiveness of wrist manipulative therapy in patients with lateral epicondylitis. Journal of Hand Therapy. Retrieved from: https://www.sciencedirect.com/science/article/pii/S0894113022000989
Jill Cook: Cardoso, T. B., Pizzari, T., Kinsella, R., Hope, D., & Cook, J. L. (2019). Current trends in tendinopathy management. Best Practice & Research Clinical Rheumatology, 33(1), 122-140. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S1521694219300233
Stasinopoulos, D., & Stasinopoulos, I. (2017). Comparison of effects of eccentric training, eccentric-concentric training, and eccentric-concentric training combined with isometric contraction in the treatment of lateral elbow tendinopathy. Journal of hand therapy, 30(1), 13-19.Retrieved from: https://www.sciencedirect.com/science/article/pii/S0894113016301302
Shiri, R., Viikari-Juntura, E., Varonen, H., & Heliövaara, M. (2006). Prevalence and determinants of lateral and medial epicondylitis: a population study. American journal of epidemiology, 164(11), 1065-1074. Retrieved from: https://academic.oup.com/aje/article/164/11/1065/61970?login=false