Tingling, numbness, burning or sharp/electric pain to the forearm or hand are relatively common symptoms. This may indicate a nerve compression problem. A nerve that is not functioning well or conducting messages properly might be swollen, stretched or void of blood supply. If you have ever had any tingling or numbness in the hand you may have found yourself instinctively shaking your arm. This action is actually just bringing more blood supply to the nerve and making it happier again. The action often provides temporary relief only.
Carpal tunnel syndrome is one of those conditions that is caused by compression or swelling of a nerve. It also one of the most widely documented conditions in the body and typically associated with tingling and numbness in the thumb, index and middle fingers (Charles et al., 2009). However, there are actually many more conditions that might be related to your tingling, numbness and burning especially if those symptoms are a little vaguer and more widespread throughout your arm.
A diagnosis might be quite straightforward or potentially very tricky. With a plethora of information available on the web there is an increasing tendency in our practice for patients to be self-diagnosing. Whilst this sometimes proves to be very accurate, it sometimes isn’t. We also see patients that may have had several treatments for a particular nerve problem such as carpal tunnel syndrome and it turns out being something totally different. This actually happens quite a bit in medicine and having a supportive and collaborative treatment team is usually essential to get a definitive diagnosis of a challenging problem. Unfortunately, the process can be time consuming, costly and frustrating.
Let’s start by exploring some common causes of a nerve compression problems in the hand or arm:
Possible causes of neural compression in the hand and arm may include:
Whilst there are several different nerve conditions in the forearm, this blog will focus on pronator syndrome which could easily be mistaken for carpal tunnel syndrome.
Both carpal tunnel syndrome and pronator syndrome involve compression of the same nerve, called the median nerve. These conditions are differentiated by the site where the nerve is compressed and are named accordingly. Symptoms and management of each of these conditions will differ due to this different level where the nerve is affected.
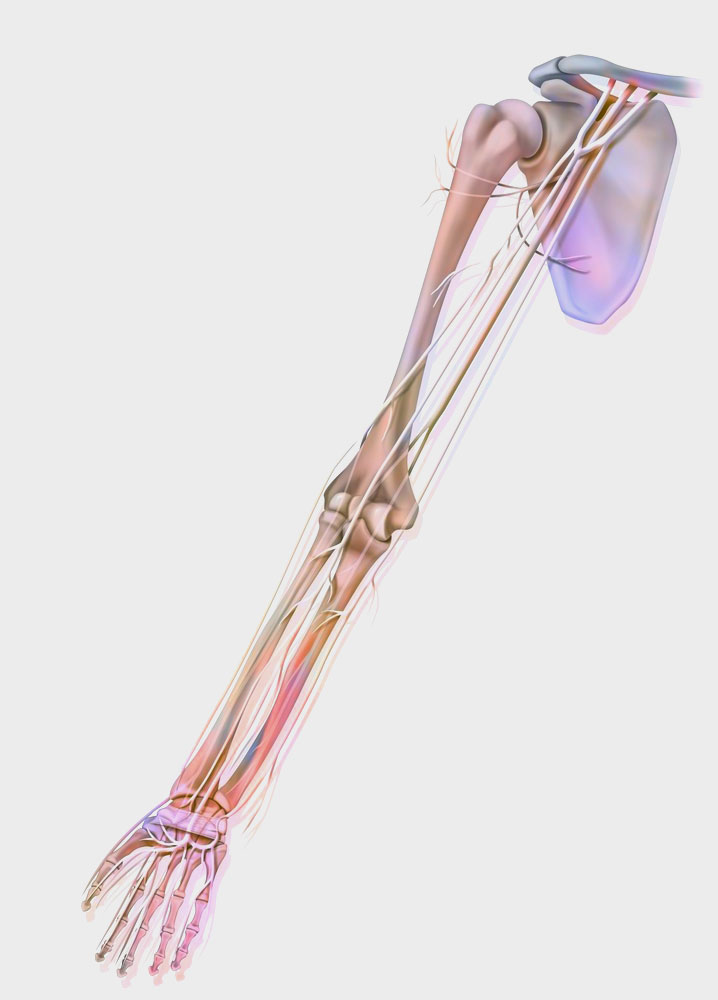
To better understand this concept, let’s have a better look at the Median Nerve and where it travels in the arm.
The median nerve is one of primary nerve branches of the arm providing motor and sensory input to both the hand and parts of the forearm. This nerve is formed by a collection of nerve fibres from the spinal cord which converge at the region of the shoulder known as the brachial plexus. The median nerve travels down the front of the upper arm alongside the brachial artery and biceps. It then travels across the front of the elbow, and into the forearm. In the forearm it sits between the muscles that bend our fingers. At the forearm level it has branches that send signals to and from some of our forearm muscles to help with movement. This is referred to ‘motor’ function.
The nerve also has a ‘sensory’ function as well which helps to feel touch, temperature and pressure. As it passes through the wrist and carpal tunnel it then branches out to the thumb index, middle fingers.
FACT: Compression sites for the median nerve occur most frequently between the elbow and hand (Alder & Wolf, 2020).
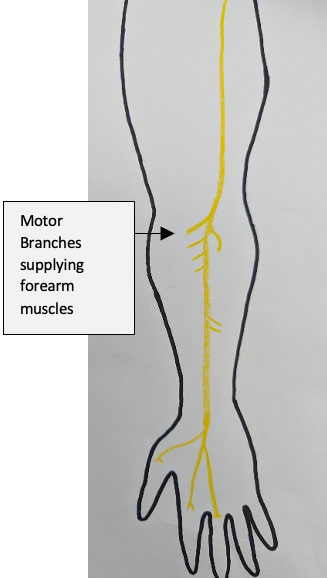
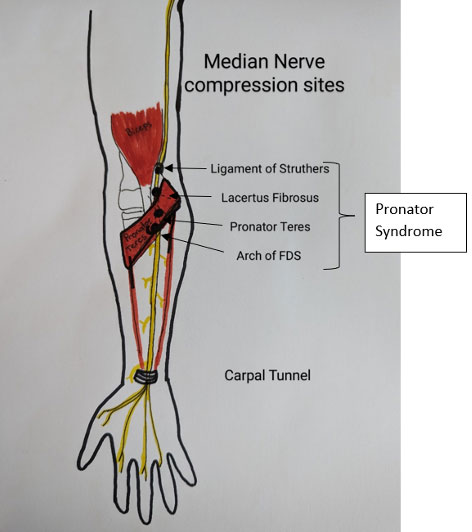
A compression at any one of the above sites is collectively known as Pronator Syndrome.
Fact: A motor branch of the median nerve, called the Anterior Interosseus Nerve separates just below the elbow near the pronator teres muscle. In some instances compression to this smaller nerve can occur, contributing to difficulties and weakness with pinching of the thumb and index finger
People with Pronator Syndrome often describe a deep aching or sharp pain radiating down their forearm with altered sensation to the hand.
Symptoms are usually worsened by similar actions to carpal tunnel, including repeated wrist motion or prolonged wrist flexion (bending), however may also be worsened in sustained or repeated palm down forearm postures. Clients usually find actions such as using a mouse or holding their mobile phone to the ear quite uncomfortable and fatiguing.
Fact: People who engage in regular forearm twisting activities or present with enlarged or tight forearms are more likely to develop Pronator Syndrome due to pressure on the nerve by the pronator teres muscle (Alder & Wolf, 2020.)
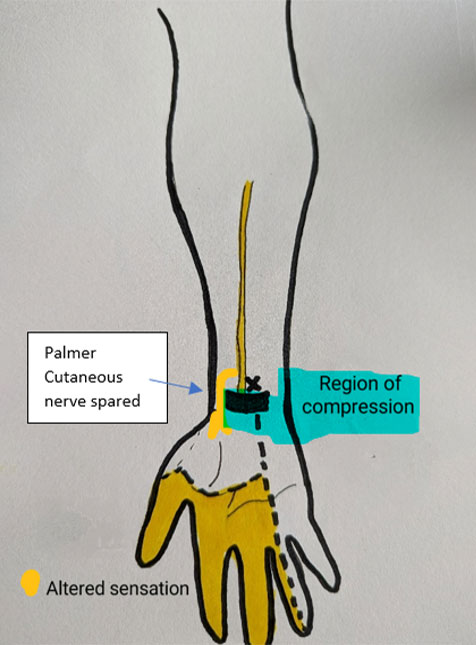
Whilst symptoms of pronator syndrome can be quite similar to carpal tunnel syndrome, a distinguishing symptom of pronator syndrome is the area of which sensation is affected. In cases of pronator syndrome, the region of the base of thumb and palm will typically present with altered sensation. This is compared to carpal tunnel syndrome where sensation to the base of the thumb is usually normal. The reasoning for this is due to the separation of a small sensory nerve, called the palmer cutaneous nerve which sits outside the carpal tunnel. In carpal tunnel syndrome the nerve is compressed in the tunnel and therefore messages that transmit before the tunnel function normally. The following pictures demonstrate this more clearly:
Pronator Syndrome
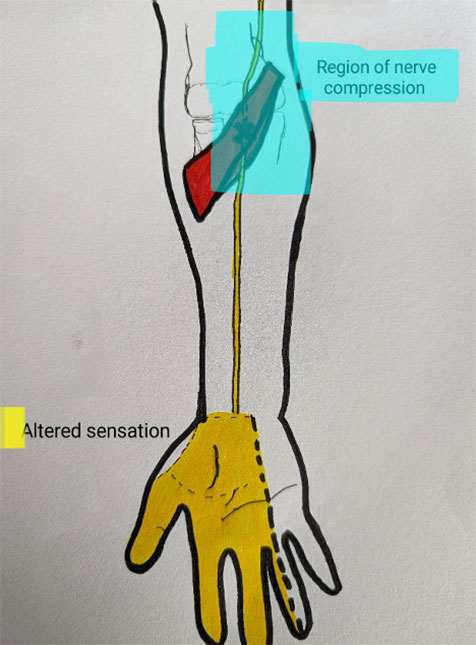
Carpal Tunnel Syndrome
Pronator syndrome is a less common median nerve compression, particularly when compared to carpal tunnel syndrome. However due to both conditions sharing similar symptoms, it is possible many cases are not detected. This idea is supported by literature. One such study of 90 people with carpal tunnel type symptoms were investigated, with 5.6% having symptoms more consistent with pronator syndrome (Saba and Sulton, 2014). The occurrence of both syndromes is also noted in similar studies with 21 of 344 cases identified with both carpal tunnel and pronator syndrome when investigated surgically (Hsiaoa, Shiha and Hung, 2017).
A nerve conduction study provides information regarding the nerve’s conduction efficiency by stimulating the nerve and investigating for any conduction delays. This study may be recommended by your GP or specialist to assist better understanding of symptoms related to a nerve. Imaging via ultra-sound or MRI can also indicate signs of a nerve injury. These studies can be helpful to identify carpal tunnel compression, however are often unreliable in identifying pronator syndrome (Adler & Wolf, 2020).
It’s also possible that you might have symptoms of tingling and numbness despite already having had a carpal tunnel release. If the carpal tunnel has been fully released, then pronator syndrome might be one potential cause of ongoing pain and should be investigated or ruled in as a possible diagnosis.
Careful consideration and monitoring of the patterns of your symptoms via hand therapy assessment and treatment can assist pathways for diagnosis. This may include a trial period of activity modification strategies or a period of splinting to reduce surrounding muscle tension. Specific exercises in an effort to increase the nerves health and mobility are also often helpful.
Most causes of pronator syndrome will resolve over a 3–6-month period, with assistance of management strategies; which as stated above may include, nerve mobility exercises, local treatment, splinting and postural supports to reduce pressure on the nerve (Adler & Wolf, 2020; Akhondi, 2022). In some cases surgical options may be considered.
SA Hand Therapy can review your symptoms to assist pathways to diagnosis and treatment, including liaising with any relevant others on your treating team to share assessment findings and ongoing recommendations for treatment of your symptoms.
References:
Adler, J. A., & Wolf, J. M. (2020). Proximal median nerve compression: pronator syndrome. The Journal of Hand Surgery, 45(12), 1157-1165. https://doi.org/10.1016/j.jhsa.2020.07.006
Charles, J., Fabridin, S., Britt, H. (2009). Carpal Tunnel Syndrome. Australian GP Statistics & Classification Centre, University of Sydney, NSW. 38(9). Retrieved from: https://www.racgp.org.au/getattachment/9a59f4ba-3cd5-4640-8f9e-b92ac1631800/Carpal-tunnel-syndrome.aspx
Hsiao, C. W., Shih, J. T., & Hung, S. T. (2017). Concurrent carpal tunnel syndrome and pronator syndrome: a retrospective study of 21 cases. Orthopaedics & Traumatology: Surgery & Research, 103(1), 101-103. https://doi.org/10.1016/j.otsr.2016.10.009
Knutsen, E. J., & Calfee, R. P. (2013). Uncommon upper extremity compression neuropathies. Hand clinics, 29(3), 443-453.https://doi.org/10.1016/j.hcl.2013.04.014
Sos, C., Roulet, S., Lafon, L., Corcia, P., Laulan, J., & Bacle, G. (2021). Median nerve entrapment syndrome in the elbow and proximal forearm. Anatomic causes and results for a 55-case surgical series at a mean 7 years’ follow-up. Orthopaedics & Traumatology: Surgery & Research, 107(2), 102825. https://doi.org/10.1016/j.otsr.2021.102825